Calming airway inflammation starts with understanding triggers, medications and daily habits that protect your lungs, ease breathing discomfort and reduce future flare ups. Maybe you live with asthma, chronic bronchitis or simply feel breathless every winter. You are not alone, and small adjustments can bring surprisingly noticeable relief over time. In this guide, we will walk through practical ways to ease that irritation. We will keep the explanations simple while still grounded in recognised respiratory medicine principles. Think of it as a friendly briefing before you talk with your own doctor.
What does airway inflammation actually mean?
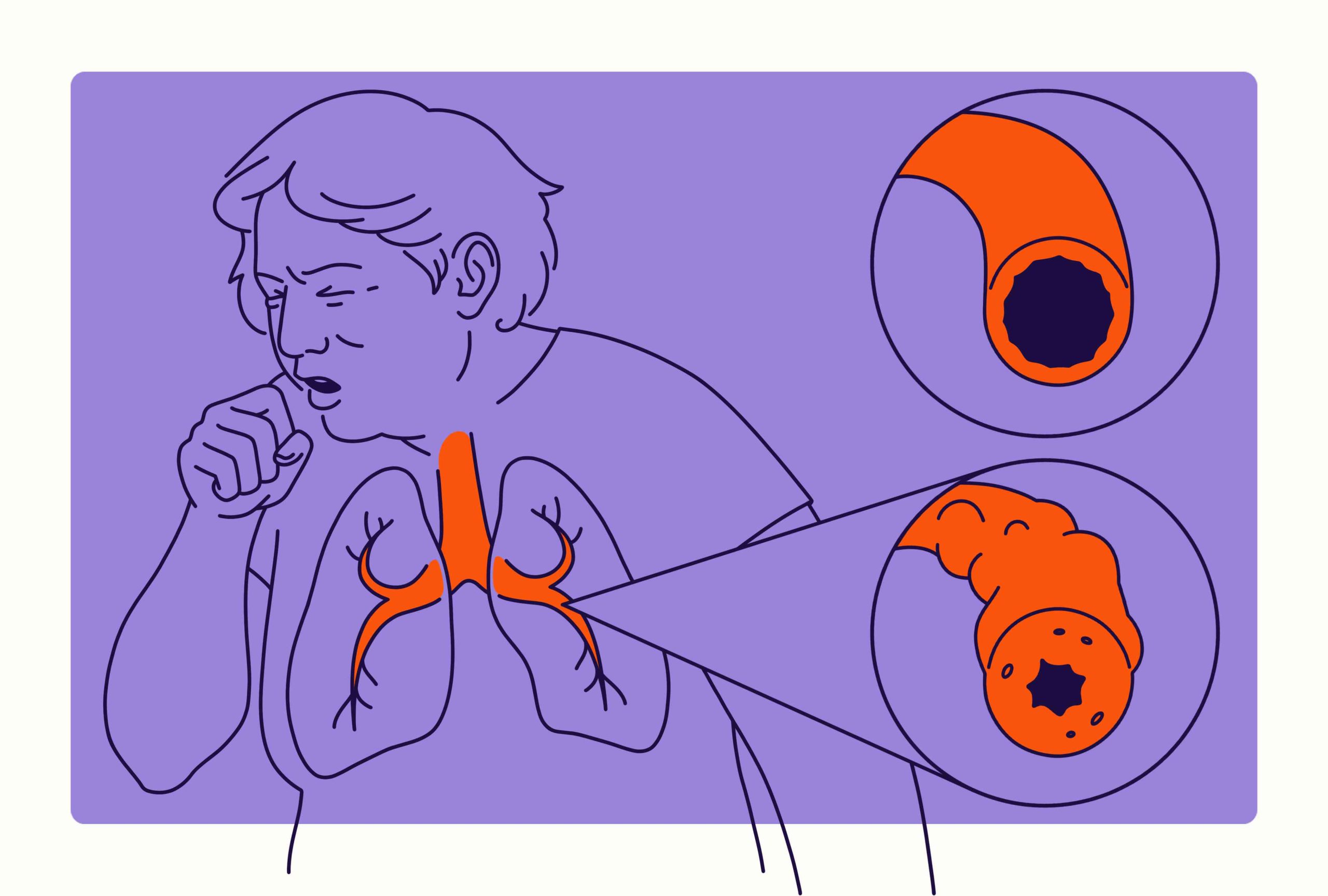
When doctors talk about airway inflammation, they usually mean swelling inside the breathing tubes. These tubes run from your nose and mouth down into your lungs. Their lining can become swollen, red and more sensitive than usual. The muscles around the airways may also tighten, making the passage even narrower. Extra mucus often appears, which can clog already narrowed spaces. All of this together makes air move less easily in and out. You might then notice cough, wheeze, tightness or a feeling that breathing takes more effort. According to our editor’s research, people often underestimate this inflammation because it is not visible from outside.
Which triggers commonly irritate the airways?
Different people react to different triggers, but some patterns appear again and again. Cold air, cigarette smoke and strong chemical fumes are frequent irritants. Dust mites, pollen, pet dander and mould can spark inflammation in sensitive lungs. Respiratory infections like colds and flu temporarily inflame the airway lining as they spread. Exercise can trigger symptoms in some people, especially in cold or dry environments. Reflux from the stomach can also irritate the throat and lower airways over time. As a result of our editor’s reviews, keeping a simple symptom diary often helps track personal triggers more clearly. Once you know your main triggers, you can focus your energy on the most relevant changes.
How do anti inflammatory medicines calm the airways?
Many treatment plans start with inhaled corticosteroids, which are the main anti inflammatory medicines for asthma. These drugs work directly on the airway lining to reduce swelling and sensitivity. They are taken in low doses through inhalers, so their effect is mostly local. Over time, regular use can make the airways less reactive to everyday triggers. Some patients also receive combination inhalers that include both a steroid and a long acting bronchodilator. The bronchodilator relaxes the muscles around the airways, while the steroid calms the underlying inflammation. For flare ups, short courses of steroid tablets may be prescribed, but doctors use these carefully because of possible side effects. According to our editor’s research, sticking to the prescribed inhaled routine is one of the strongest predictors of stable control.
Why inhaler technique matters more than many people think
Even the best medicine cannot work if it does not reach the lungs properly. Poor inhaler technique is surprisingly common, across all age groups and backgrounds. People forget to shake the canister, breathe at the right speed or hold their breath afterward. Some breathe in through the nose instead of the mouth without realising it. Others stop using a spacer even though it previously improved delivery. These small mistakes can mean that much of the medication stays in the mouth or throat. According to our editor’s research, regular technique checks during clinic visits can raise the real dose reaching the lungs without changing the prescription. It is always reasonable to ask your doctor or nurse to watch you use your inhaler and offer small corrections.
Lifestyle choices that support calmer airways
Medication is important, but everyday habits can either support or undermine its effect. Not smoking is the single most powerful step for airway health. Avoiding second hand smoke and heavy pollution exposure is also crucial whenever possible. Regular, moderate exercise helps improve overall lung capacity and strengthens breathing muscles. For many people, gentle walking or cycling is enough to start. Maintaining a healthy weight can reduce breathlessness, because excess weight presses on the lungs and diaphragm. According to our editor’s research, people who combine medication with these lifestyle steps often report fewer flare ups and better stamina. Small, steady changes usually work better than drastic, short lived efforts.
How can you adapt your home environment?
Your home environment can quietly shape daily inflammation levels. Simple measures such as regular vacuuming and washing bedding at higher temperatures help reduce dust mites. Keeping indoor humidity in a balanced range can discourage mould growth. Pet owners may need to keep animals out of the bedroom, especially if allergy tests confirm sensitivity. Strong cleaning sprays, scented candles and air fresheners can all irritate delicate airways. Using milder, fragrance free products often makes a noticeable difference. As a result of our editor’s reviews, many patients only realise the impact of these factors after they experiment with small, targeted changes at home. The goal is not a perfect environment, but a kinder one for your lungs.
Managing infections without worsening inflammation
Viral infections are a common cause of airway flare ups, especially during colder seasons. Good hand hygiene, vaccination where recommended and avoiding close contact with sick people all reduce risk. When you do catch a cold, early use of your personalised action plan becomes important. Some patients have instructions to increase inhaler doses for a few days after symptoms start. Rest, fluids and simple pain relief support the body while it fights the infection. It is important not to suddenly stop maintenance inhalers during mild illnesses unless a doctor advises this. According to our editor’s research, stopping control medication abruptly can leave the airways unprotected just as they face fresh viral irritation. Knowing when to seek medical review during an infection is also part of your plan.
What role does allergy control play?
For many people, airway inflammation is closely tied to allergies. In those cases, controlling allergy exposure and symptoms can reduce ongoing swelling. Antihistamine tablets, nasal sprays and allergen avoidance all have roles. For example, managing hay fever well can ease both nasal and chest symptoms. Some patients benefit from allergy testing to clarify which substances matter most. In carefully selected cases, desensitisation treatments may be discussed with specialists. According to our editor’s research, coordinated care between allergy and respiratory teams tends to produce better control than treating each area separately. Paying attention to both nose and chest often gives the lungs a quieter daily background.
When should you seek medical advice quickly?
Certain warning signs mean you should not simply wait and see. Needing your quick relief inhaler much more often than usual is one of them. Struggling to speak full sentences without pausing for breath is another important sign. Blue lips, severe chest tightness or a feeling of heavy suffocation are emergencies. Waking repeatedly at night with breathlessness also deserves prompt review. If a child is using their chest and neck muscles heavily just to breathe, urgent assessment is needed. According to our editor’s research, early medical help during a flare can prevent hospital admission and reduce long term damage. It is safer to ask for help too early than too late.
Working with your healthcare team over time
Airway inflammation is often a long term condition rather than a quick visitor. That means regular follow up usually brings better results than occasional crisis visits. During reviews, your doctor can adjust medication, check inhaler technique and discuss new symptoms. You can share concerns about side effects, lifestyle changes and future plans, such as travel or sports. Together, you can refine an action plan that feels realistic for your daily life. According to our editor’s research, patients who feel involved in decisions are more likely to follow through on agreed steps. Over time, this partnership can turn a frustrating condition into something more predictable and manageable.