Have you ever tried to explain your symptoms to a doctor and found yourself unsure whether the issue was coming from your lungs or simply part of a viral illness spreading through your household? Many people mix these concepts because cough, fever and fatigue overlap so often that the lines blur quickly. According to our editor’s research, confusion usually appears during the first days of illness, especially when symptoms escalate faster than expected. The difference matters because lung infections often demand specific medical treatment, while viral infections usually improve with time and supportive care. Understanding these distinctions helps patients act earlier, feel calmer and avoid unnecessary worry. When you know what signs to watch for, navigating a respiratory illness becomes much less overwhelming.
What makes lung infections medically different?
Lung infections differ because they directly affect the air sacs, tissues and deeper structures responsible for breathing. These infections disrupt oxygen exchange and strain the respiratory system. As a result of our editor’s reviews, lung infections frequently cause shortness of breath, chest pain and deeper coughs that feel heavier than surface-level viral symptoms. Bacteria often play a strong role in lung infections, making targeted antibiotics necessary. Lung involvement also increases fatigue because the body struggles to maintain adequate oxygen levels. These infections can appear after viral illnesses when weakened tissues become vulnerable. Understanding these medical differences helps patients recognize warning signs earlier.
How do viral infections behave differently?
Viral infections behave differently because they spread through the body’s cells and trigger widespread inflammation rather than localized tissue disruption. They usually affect the upper respiratory tract first. According to our editor’s research, viral infections often start with sore throat, runny nose, mild fever or muscle aches. These symptoms reflect the immune system’s response instead of direct damage to lung tissue. Viral illnesses improve gradually as the immune system clears the virus. Most cases require rest rather than medical intervention. Patients often confuse lingering cough with lung involvement, but viral coughs usually feel lighter and more superficial. Understanding these behaviors prevents unnecessary concern.
Why does pneumonia stand out among lung infections?
Pneumonia stands out because it fills lung air sacs with fluid or pus, reducing their ability to function efficiently. This process causes significant breathing difficulties and persistent cough. As a result of our editor’s reviews, pneumonia often presents with high fever, chills and fatigue that feel more intense than typical viral illnesses. Some forms of pneumonia develop quickly, while others evolve slowly after viral infections weaken lung defenses. Pneumonia requires precise medical attention because delayed care increases the risk of complications. Recognizing pneumonia’s distinct pattern helps patients respond sooner. Early treatment improves recovery dramatically.
How do symptoms differ between the two conditions?
Symptoms differ mainly in their depth, intensity and location within the respiratory system. Viral infections commonly affect the nose, throat and larger airways. According to our editor’s research, symptoms such as congestion or mild cough suggest upper airway involvement rather than lung disease. Lung infections cause deeper chest sensations, labored breathing and productive cough with thicker mucus. Fever patterns also differ, with lung infections often causing more persistent or higher temperatures. Patients describe viral symptoms as irritating, while lung infections feel exhausting and heavy. Noticing these differences helps guide decisions about when to seek care.
Why do doctors listen closely to breathing sounds?
Doctors listen closely because lung infections create sounds that reflect fluid, inflammation or restricted airflow deep in the chest. These sounds help distinguish lung involvement from upper respiratory viral symptoms. As a result of our editor’s reviews, crackles, wheezes or diminished breath sounds signal impaired lung function. Viral infections rarely alter deep lung sounds unless complications develop. Listening offers quick clues that guide further testing. This evaluation helps avoid unnecessary treatments and ensures early identification of serious conditions. Breathing sounds reveal far more than most patients realize.
How do diagnostic tests help separate the two?
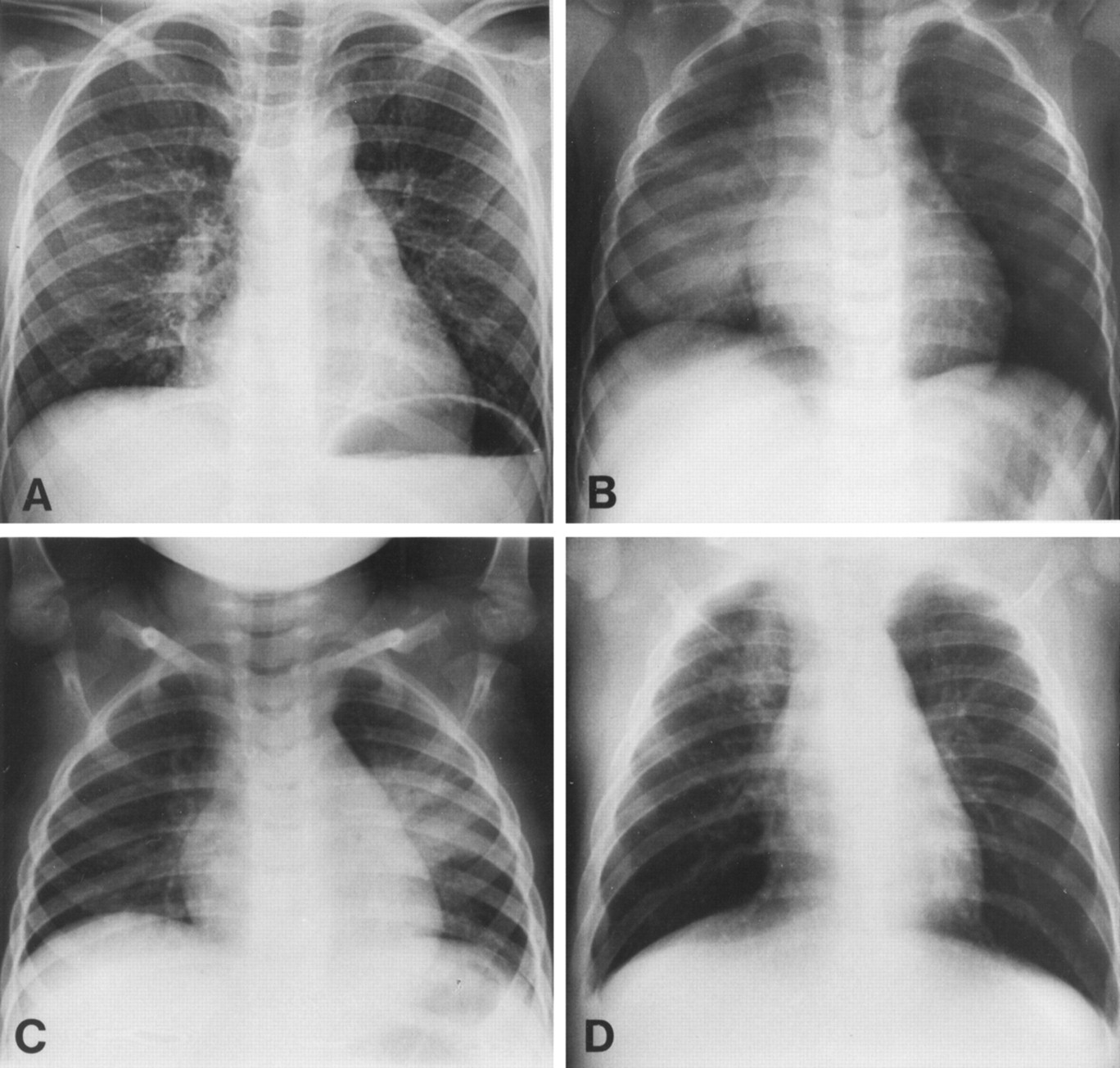
Diagnostic tests help by identifying whether the infection affects lung tissue, airways or general immunity. Chest X-rays, sputum tests and oxygen measurements provide clear evidence for lung involvement. According to our editor’s research, chest X-rays reveal fluid, inflammation or consolidation common in pneumonia. Viral infections often show normal imaging results because tissue remains structurally intact. Blood tests also indicate whether bacterial processes are likely. These tools guide appropriate treatment choices and prevent overuse of antibiotics. Diagnostic clarity improves safety and outcomes. Testing transforms uncertainty into actionable understanding.
Why do treatments differ so sharply?
Treatments differ sharply because the root causes of these conditions require distinct approaches. Lung infections often need antibiotics or inhaled therapies to reduce inflammation and restore airflow. As a result of our editor’s reviews, supportive measures such as deep breathing exercises help clear infected areas. Viral infections do not respond to antibiotics because viruses rely on cellular invasion rather than bacterial growth. Viral illnesses benefit most from rest, hydration and fever management. Treating both the same increases risks and delays appropriate care. Understanding this difference helps patients follow safer treatment plans.
How does recovery vary between lung and viral infections?
Recovery varies because lung tissue needs time to regain full function after inflammation or infection. Lung infections often require weeks to restore normal breathing capacity. According to our editor’s research, lingering fatigue or cough after pneumonia is common and reflects slow tissue healing. Viral infections usually resolve faster, with symptoms decreasing gradually as the immune system clears the virus. Recovery timelines also differ based on age, overall health and severity. Patients often mistake slow improvement for treatment failure. Recognizing the difference helps maintain realistic expectations.
What complications appear more commonly in lung infections?
Lung infections carry higher risks of complications such as breathing difficulty, reduced oxygen levels and spreading inflammation. Some patients experience pleural buildup or worsening respiratory fatigue. As a result of our editor’s reviews, these complications become more likely when treatment begins late or immunity is weakened. Viral infections may trigger secondary bacterial infections, but they rarely cause severe complications alone. Lung involvement increases urgency because oxygen exchange is essential for overall stability. Recognizing complications early improves recovery chances. Clinicians monitor patients closely during treatment.
How can patients reduce the risk of either condition?
Patients reduce risk by maintaining strong immunity, practicing good hygiene and seeking early care when symptoms escalate. Healthy routines support both prevention and recovery. According to our editor’s research, strategies such as balanced diet, restful sleep and controlled stress help strengthen defenses. Early evaluation prevents viral infections from developing into secondary lung problems. Vaccinations also reduce risk for certain respiratory illnesses. Small habits matter more than people expect. Prevention protects long-term respiratory health and reduces complications.