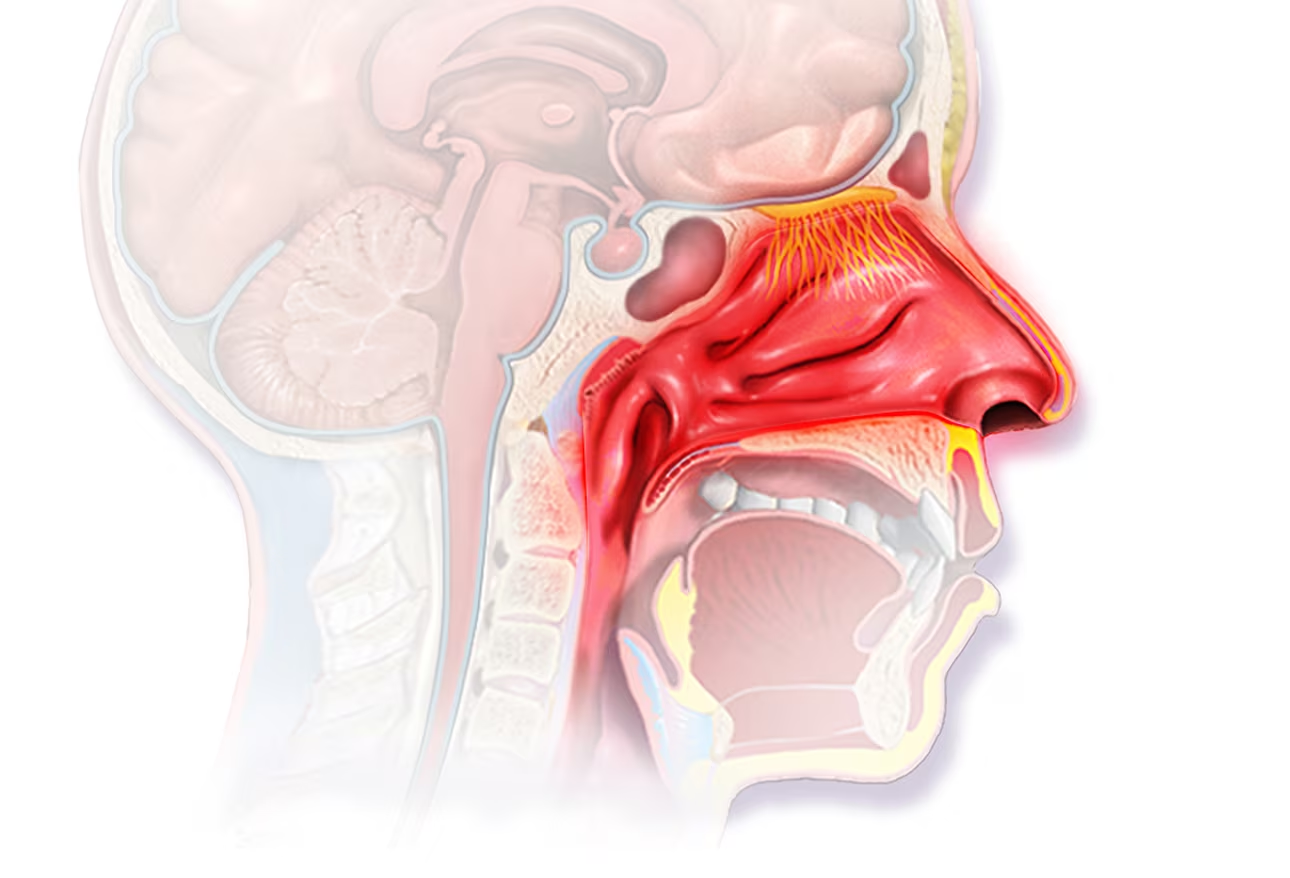
Allergic rhinitis doesn’t always feel like a lung issue. Sneezing, nasal congestion, and postnasal drip often appear before lower respiratory symptoms begin. These upper airway symptoms are often seasonal, tied to pollen or dust exposure. Many patients don’t connect nasal symptoms to deeper respiratory changes. However, inflammation in the nose can travel downward. Mucus dripping into the throat often irritates the airways. It’s not unusual for people with allergic rhinitis to experience coughing or throat clearing during flare-ups. This cycle may last weeks, sometimes unnoticed until it affects sleep or breathing comfort.
Inflammation from allergic triggers can extend into the bronchial passages over time
The connection between sinuses and lungs isn’t abstract. Inflammation from allergic triggers can extend into the bronchial passages over time. When allergens enter through the nose, they don’t always stay there. The same immune cells reacting in the sinuses can activate in the lungs. This shared pathway explains why some people develop asthma-like symptoms alongside allergies. Breathing may feel shallow or effortful during high pollen periods. Even without wheezing, chest tightness can develop. Over time, repeated episodes can reduce lung efficiency. Ignoring mild shortness of breath may allow deeper inflammation to build unnoticed.
People with allergic rhinitis often report chest discomfort during allergy season
Symptoms don’t always stay in the nose. People with allergic rhinitis often report chest discomfort during allergy season. They describe it as tightness or occasional shortness of breath, especially during activity. For some, it’s worse in the morning or after spending time outdoors. This is not always asthma, but irritation in the bronchial lining. Airways become more sensitive to temperature, pollutants, or exercise. Those with long-standing allergic rhinitis are more likely to experience these lower airway effects. Monitoring breathing changes during allergy season is essential, even in the absence of wheezing.
Chronic nasal blockage may lead to mouth breathing, affecting oxygen intake and lung comfort
Nasal congestion can change how we breathe. Chronic nasal blockage may lead to mouth breathing, affecting oxygen intake and lung comfort. The nose filters and humidifies air, preparing it for the lungs. Mouth breathing bypasses this process, delivering drier and colder air directly. This can irritate bronchial tubes and increase coughing. Overnight, it may lead to poor sleep quality and daytime fatigue. Some people snore or experience dry mouth frequently. These signs may point to hidden respiratory strain linked to allergic congestion. The shift from nasal to oral breathing has consequences beyond comfort.
Recurrent allergies may prime the lungs for future reactive airway responses
Allergy symptoms don’t exist in isolation. Recurrent allergies may prime the lungs for future reactive airway responses. Every allergic reaction increases immune sensitivity, lowering the threshold for future flare-ups. With time, even mild triggers can provoke intense responses in both the nose and lungs. Coughing fits, chest tightness, or activity intolerance may develop without infection. Lung tissues, once inflamed repeatedly, become less tolerant to normal air pollutants. What begins as seasonal rhinitis can shift into chronic respiratory sensitivity. This pattern is more common than many assume, especially in early adulthood.
Nasal sprays help relieve congestion but don’t always address deeper respiratory inflammation
Topical treatments provide short-term relief. Nasal sprays help relieve congestion but don’t always address deeper respiratory inflammation. Decongestants shrink swollen vessels but don’t block systemic allergic reactions. Steroid sprays reduce inflammation, but their effects stay mostly in the upper airway. Antihistamines may dry secretions but do little for chest symptoms. Those with lung discomfort often need broader allergy management. Inhalers, leukotriene blockers, or immunotherapy may be required for full control. Treating only nasal symptoms may leave bronchial inflammation unchecked. A comprehensive approach becomes necessary when both upper and lower symptoms exist.
Environmental control reduces exposure and supports both nasal and lung health
Reducing allergen contact remains a key strategy. Environmental control reduces exposure and supports both nasal and lung health. Air purifiers, HEPA filters, and regular dust removal reduce indoor triggers. Avoiding outdoor activity during high pollen hours helps prevent flare-ups. Changing clothes and showering after outdoor exposure removes particles from skin and hair. Keeping bedroom windows closed during allergy season protects overnight breathing. These steps benefit lungs and sinuses equally. Many patients improve significantly with consistent environmental control alone. However, results depend on discipline and routine—not occasional effort.
Undiagnosed allergic rhinitis may mimic asthma or chronic bronchitis over time
Some diagnoses overlap subtly. Undiagnosed allergic rhinitis may mimic asthma or chronic bronchitis over time. Persistent coughing, wheezing, or chest tightness often leads to misdiagnosis. If lung tests show minimal obstruction, allergies may be the root cause. Many patients are treated for asthma when nasal allergies are driving symptoms. Identifying postnasal drip or night coughing helps clarify the origin. Diagnostic clarity matters when prescribing long-term medications. Mislabeling leads to unnecessary inhaler use or missed allergy management. Careful questioning often reveals overlooked rhinitis symptoms in chronic cough cases.
Children with nasal allergies are more likely to develop lung sensitivity later in life
The pattern often starts young. Children with nasal allergies are more likely to develop lung sensitivity later in life. Early exposure to allergens trains the immune system to overreact. Repeated nasal inflammation increases vulnerability in the lungs. School-aged children with frequent congestion often begin coughing during sports or in cold air. If untreated, this can evolve into reactive airway symptoms by adolescence. Pediatric allergy care helps reduce long-term respiratory risk. Early intervention with antihistamines or allergy shots may change the trajectory of lung health. Recognizing these links helps parents take proactive steps early.
Lung function may decline silently if allergic rhinitis remains uncontrolled for years
Respiratory changes aren’t always dramatic. Lung function may decline silently if allergic rhinitis remains uncontrolled for years. Shortness of breath may be mistaken for poor fitness. Activity avoidance becomes habitual, further reducing capacity. Inflammation spreads slowly and painlessly across tissues. By the time symptoms are recognized, function may be significantly reduced. Routine pulmonary function testing is rarely offered in allergy care. Those with frequent rhinitis episodes should request evaluation, especially if exercise feels harder. Catching the decline early makes reversal more likely. Waiting often leads to missed recovery opportunities.
Combining allergy management with pulmonary care improves both outcomes and quality of life
Care should cross specialties. Combining allergy management with pulmonary care improves both outcomes and quality of life. Allergists focus on identifying and desensitizing triggers. Pulmonologists address airflow, inflammation, and lung capacity. When the two work together, treatment is more precise. Patients with both nasal and lung symptoms benefit from integrated care plans. Medications can be streamlined, and redundant therapies avoided. This collaboration becomes critical when symptoms affect sleep, work, or school. Treating just one area often leaves the other untreated. A broader approach reduces relapse and improves daily function.
Patients often recognize improvement only after airflow is restored across the entire system
Breathing issues evolve slowly. Patients often recognize improvement only after airflow is restored across the entire system. Treating nasal passages alone may help for a while. Adding lung-focused therapies often reveals hidden discomfort. Energy improves, sleep deepens, and physical activity becomes easier. These changes happen gradually. Many patients don’t realize how restricted their breathing was until it improves. Allergic rhinitis masks deeper symptoms by focusing attention on the nose. When both systems are open, breathing feels smoother and more natural. This shift is often subtle—but transformative.
Source: Pulmonology in Dubai / Pulmonology in Abu Dhabi